Innovating the Patient Experience
On the Road with OpenLab at University Health Network – August 2015
by Jason Wolf
The OpenLab Story
Our latest On the Road took us to the bustling streets of Toronto, Ontario, Canada and out of the typical halls of direct care to the critical consideration of how innovation and improvement can and should play a role in patient experience. My visit was with OpenLab, a design and innovation shop dedicated to finding creative solutions that transform the way health care is delivered and experienced. OpenLab was born from the historic work of UHN’s Centre for Innovation in Complex Care (CICC) just late last year.
CICC was founded six years ago on a simple idea – to use the general internal medicine ward at Toronto General Hospital as a living laboratory for experimenting with new ways to improve care for complex patients. Over time, their work expanded into new and exciting areas and they recognized that in order to tackle the big challenges facing health care and to design solutions that naturally scale, their laboratory needed to be the health system itself.
To address this shift in thinking OpenLab established three distinct but inter-related labs to focus our work on areas where we think we can make an impact:
- Complex Care Lab – reinventing care for people with chronic disease
- Experience Lab – looking at ways to dramatically improve how people experience care
- X-Lab – exploring fresh ideas and perspectives on the future of the health system
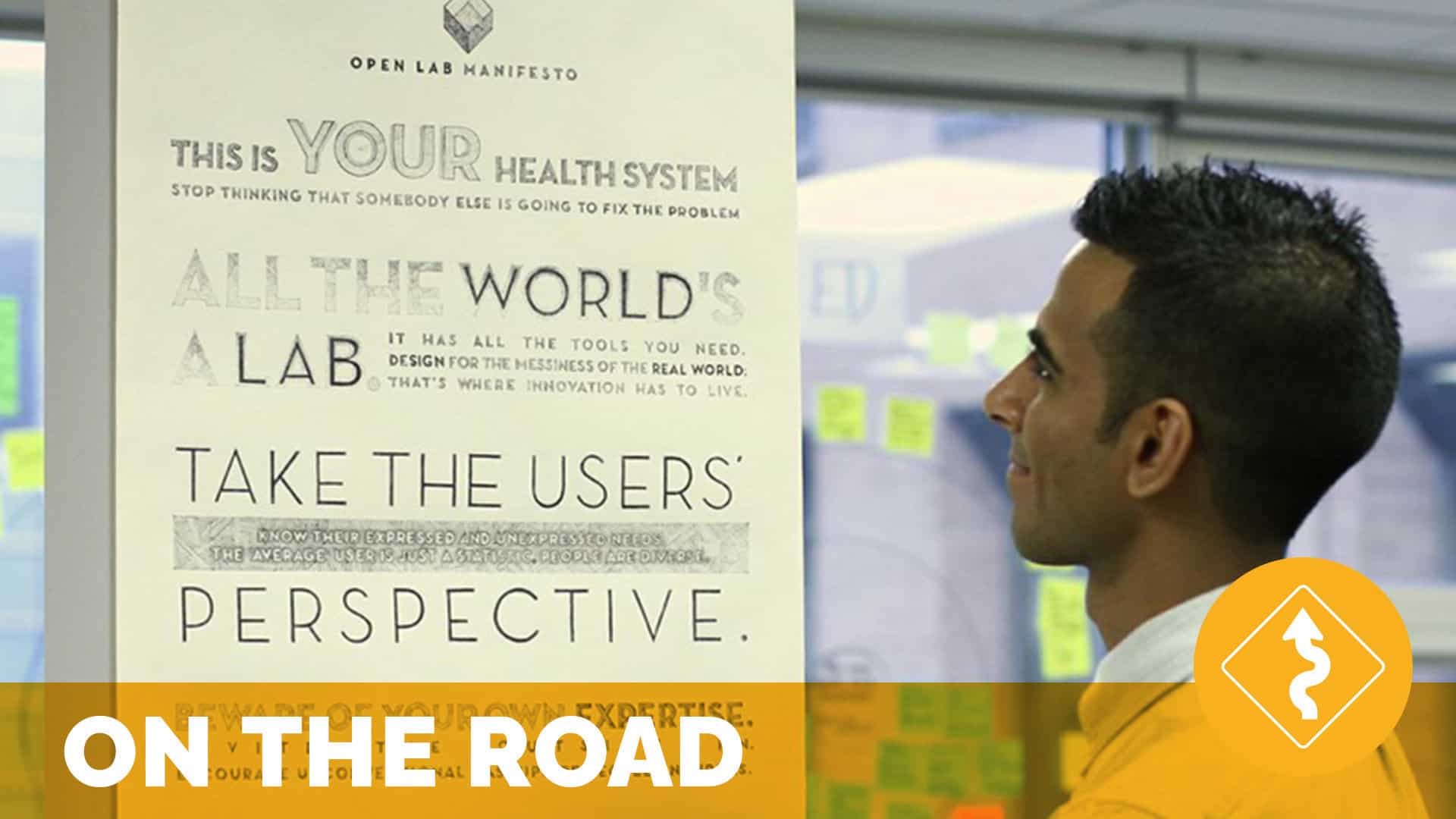
I was particularly inspired by the organization’s manifesto, pictured below, that was actually penned by hand by one of the team members. It may perhaps be the simple, yet powerful messages here that are the most significant takeaway from my visit, for while the exploration of innovative and impactful practices are critical, the mindset and framing to achieve those efforts are foundational to any success.
Key tenets of the manifesto include:
- Stop thinking somebody else is going to fix the problem
- All the world’s a lab
- Take the user’s perspective
- Beware of your own expertise, invite the outside in
- Innovate responsibly, don’t reinvent the wheel, simplicity spreads
These resounded with me for many reasons, but what was remarkable in being introduced to these ideas and then seeing them in action in all OpenLab is looking to tackle, I felt many of the same principles in play in what has enabled The Beryl Institute to rapidly grow a collaborative community and home for the patient experience movement itself.
My time with the team introduced me not only to some great ideas, but a process central to improvement efforts and simple enough to be accessible to everyone, I will share just some of the ideas here, but share here now and will reinforce as we close, that it is worth finding time to connect with the OpenLab team if you are looking for the means to innovate in your own organization.
The Work of OpenLab
My visit with OpenLab provided me a comprehensive review of a number of active and engaging programs on which the organization was working. While I will not share all here, I look to address two major considerations. The first, that we all have the opportunity to use our own organizations as centers for innovation with the right frame of reference and commitment and the second, that through exploring some of the efforts underway, we begin to see the value of true process review, collaboration and inclusion in efforts to address the improvement of experience for those in healthcare.
The power of Innovation
In my conversations with my host Shoshana Hahn-Goldberg and members of the team, including center co-founder Dr. Howard Abrams, the premise of OpenLab was presented as both rigorous, yet profoundly simple. Dr. Abrams shared that “there was a realization that one, we had a living breathing laboratory to understand what was (and was not) working in providing the best in care, outcomes and overall experience for our community and we had an organization comprised of potential innovators who have the ideas, the knowledge and the ability to contribute that was untapped.” When I think about this description, I can’t help but see this in many of the healthcare organizations that exist today, yet transactional change leads the day and process improvement efforts more often redesign problems versus innovate for lasting solutions. The OpenLab process was meant to combat this.
In term of the work of OpenLab, as new ideas emerge, they are vetted, prioritized and then added to the work plan. With no more than 10-15 projects being conducted at any one time, on 6-week improvement cycles and grounded in solid improvement methodology, the organization is not beholden to linear thoughts, but rather has compiled an impressive team of broad and varied thinkers to begin to poke and prod at the working issues.
To add to the expansion of ideas, OpenLab reinforces its name with a process called “Open Rounds”. As described, open rounds are exactly what they say. The rounds, which are actually an open session where current projects are reviewed by their project lead and new ideas are pitched and explored, are open for everyone to attend, not just from the organization, but the community at large. Open Rounds are held weekly and are often attended by people unaffiliated with OpenLab.
These sessions return to the fundamentals shared in OpenLab’s manifesto, “invite the outside in”. This idea is counter to so much of the innovation and strategy work that takes place behind closed doors or in private meetings through which organizations seek to make improvements. There is something profoundly revealing and inspiring when you think your ideas can be tested, molded or altered by a voice you have never heard before and that your thinking is being shared openly in a way that it is ultimately available and open to changes it could not even anticipate.
These are brave processes in which PI methodology, meets the willingness to invite the unknown. This not only serves as a check on the process, but also allows for more voices and minds to contribute to the overall efforts taking place within the organization itself.
I would share here that for all the talk of the need for innovation in experience improvement, all too often I have seen organizations simply look to others for a new idea, be it their vendor, a consultant or even a peer organization. While these are not bad sources, they are limiting in what they can provide and from what I learned in my time with OpenLab, these efforts miss an incredible important source, the voices, thoughts and ideas of those directly involved.
This time of open innovation has led to an expansive menu of efforts across all of OpenLab’s defined lab “spaces”. While all of these programs are of incredible value (and I encourage our readers to review all current projects for how they may relate to the work you are doing or considering), I am going to share two that sit under the work of “Experience Lab” and are both focused on the potential of expanding the conversation of person centeredness in healthcare today.
Innovation in Action – Experience Lab
As described via OpenLab, “Experience Lab finds ways to dramatically improve how people experience care. This includes the patient, caregiver and provider experience. The lab uses experience and service design methods to deeply understand and respond to expressed and unexpressed needs of users.” This idea of bringing practical innovations to healthcare is not new, but yet when applied with the thoughtfulness found in OpenLab it is clear great things can happen. I will touch on two of the programs here. The first is Face 2 Name and the second is PODS.
Face2Name
The formal description of Face2Name is “a collection of studies that aims to identify the effects of providing photographs of clinicians to patients and other hospital staff on clinician anonymity, communication, and teamwork.” While not a new idea what is unique about the Face2Name effort is the rigor by which this project is being explored.
The project is much more than providing playing cards or handouts with staff pictures on it. It represents a comprehensive effort to visually connect people’s care teams with those on the receiving end of care. It is designed on a foundation of creating connectivity and building relationship in a way that links patient and care team in new and significant ways.
The program was run through clinical trials, with units receiving the information, while others did not and a great impact was realized. A great overview of the findings is presented on the Face2Name site. The “ah-has” as project lead Lora Appel shared was that aside from general awareness a true sense of connection was established in the healthcare environment that often didn’t exist. More so, there was a realized impact not just on recipients of care, but staff as well with an increase of awareness of those working around them.
Lora added, “Patients were actually surprised something like this did not exist to begin with”, which begs the question, what are we not considering such simple, yet profound interventions and resources such as this. By providing a means to help patients and families know who is caring for them, beyond just “the nurse” or “the doctor”, to who they are and what they do, has great potential for even broader impact.
The Face2Name program continues to expand its exploration now finding itself as an app for use and eventually connecting the effort to the electronic health record (EHR) as well, in which a patient’s picture can also be captured and shared with the care team. As a resource idea, many may have considered or even attempted implementation of an idea such as this before. What the OpenLab team has given us is the rationale and rigor to see this is a practice we should not be without.
PODS – Patient-Oriented Discharge Summaries
The PODs effort presents itself on the OpenLab site as follows: “The period following discharge from hospital is a vulnerable time for patients. Clearly communicating important information that patients need to know the moment they leave the hospital seems sensible, but is often not done in practice for a variety of reasons. Commissioned by the Toronto Central Local Health Integration Network (TC LHIN), OpenLab worked with patients and providers to understand unmet needs, and to co-design PODS. PODS is freely available to all organizations to adopt and adapt, based on their local circumstances.”
What was intriguing about the PODS effort was the real issue it looked to tackle. This is not only an issue in the Canadian system as we saw here, but clearly has implications for understanding of medical instructions and information impacting overall outcomes, readmissions rates and a number of other factors. Project lead Shoshana Han-Goldberg reiterated the core idea behind PODS as outlined on the PODS site, “The PODS initiative is aimed at improving the patient-centeredness of discharge through the delivery of a PODS at the time of discharge. Designed according to best practices by providers, caregivers, and patients, specifically hard-to-reach patient groups such as those with language barriers, mental health issues, and limited health literacy, PODS is easy for patients to understand and act on.”
While the design of the PODS effort was to explore the potential for a singular process, what was discovered and valuable was the need for subtle variation in the way people shared discharge information. What the efforts also showed was that here was no variance or question in the value or consideration in providing this information in a formal, documented and comprehensive manner for all leaving the care setting.
As organizations globally struggle with how to ensure effective communication on care efforts and ensure the best follow-up to ensure the best in outcomes, this process offers a significant jumping off point. The OpenLab team not only provides a comprehensive report on the value and impact of this discharge communication effort, they provide an open access toolkit and framework that I would encourage organizations to review as you look to address this issue.
The bottom line was the project team learned in the midst of all the information we provide patients and families as they leave the care setting, the most important elements include:
- Medication instructions
- Follow up appointments with phone numbers
- Normal expected symptoms, danger signs, and what to do
- Lifestyle changes and when to resume activities
- Information and resources to have handy
The PODS project exemplified the true contribution that OpenLab looks to make. As a community-focused entity committed to sharing what it learns broadly and engaging openly with the broadest range of voices, the true opportunity was exemplified not just in this project. I also saw it in all that was reinforced during my visit. We must engage the range of voices in improvement and innovation, we must broadly share our lessons learned and our programs designed in responsible ways and we must be willing to adapt our efforts to the environment, its influences and changes as we proceed. Perhaps why the lessons of the PODS project and OpenLab’s efforts overall are so appealing is that they so closely mirror our own values at The Beryl Institute. What OpenLab offers us in addition is the model by which to tackle these ideas for your own organization and perhaps for even our community globally to consider greater projects of impact moving forward.
Implications for the broader experience conversation
I would be remiss if I did not mention I had the chance to be exposed briefly to a number of incredible efforts taking place at OpenLab from engaging the broader voice of the patient, especially those facing serious illness, via the Patient Empowerment Program, to the efforts to expand the voices of individuals in the care experience through the Involve project, to an effort to explore the impact of social networks with the LifeguardRx/Mobile Feasibility Study, to an incredibly powerful effort to connect people with the health system itself, by sharing the raw view and thoughts of people – patients and care team members – through photography in the People of UHN effort. The photographs are worth the look.
The time I spent was not enough to dig into each of these efforts, but it was more than sufficient to see the work of OpenLab was driving an incredible contribution to the healthcare system, not just at UHN, but globally. By providing both a space for new thinking and the development of ideas and then the testing, reshaping and polishing of these interventions, OpenLab truly stands as a model for how the essence of innovation can (and should) be brought to any health system.
It need not be at this scale, but the efforts of OpenLab bring us back to one of our own core values at The Beryl Institute, that being innovation. We see innovation, as not just an idea, but a relentless pursuit of what we can do to impact experience. In fact, we offer it is “vigilance in continuously searching for new ways of thinking, doing and disseminating ideas.” I reassert here that it is not just looking for new ideas, but rather the intention to ensure innovation remains top of mind in impacting the experience efforts organizations are undertaking.
In a healthcare world in which the words dynamic and chaotic seem the most apt descriptors, innovation and the agility it requires at both ends is no longer an option, but rather a core competence in ensuring the best in outcomes for those impacted by our efforts. I encourage you to explore the work of OpenLab, review their projects and understand their process. Their effort can and should serve to inspire others to this work. As healthcare remains in a constant state of transformation, as demands become weightier and the voices of consumers louder, this may very well be the best strategic focus for experience and overall organizational success, not in the future, but starting today.
Thanks to Dr. Howard Abrams, my host Shoshana Han-Goldberg and the entire team from OpenLab for taking the time to share their work. Their efforts are well worth a look.
Related content
-
 Innovation & Technology
Innovation & TechnologyLaboratory Literacy: Surveying Lab Result Interpretations of a Local Patient Population
A patient’s independent interpretation of their medical laboratory data has become an unspoken prerequisite in the current age of medicine. In the outpatient setting, it is anecdotally commonplace for patients to receive their lab results before their physicians, resulting in patients often relying on self-interpretations of their results. This study analyzed the degree to which
Learn more -
 Environment & Hospitality | Innovation & Technology
Environment & Hospitality | Innovation & TechnologyThe Hospitality Effect: Creating a Culture to Improve Care & Outcomes
Elevating a great medical experience to a great patient experience means focusing on creating a great human experience. And that requires hospitality—not just in physical environments, but also in personal connections and experiences that help people feel seen and heard. Incorporating the principles of hospitality into patient care impacts the experience of patients, families, and
Learn more -
 Innovation & Technology
Innovation & TechnologyIncreasing Patient Safety with a Digital Hourly Rounding Solution
In this case study, read about how Bryan Medical Center moved from an outdated paper-based hourly rounding process to an innovative digital solution.
Learn more
