An Unwavering Commitment to the Human Experience in Action
On the Road with Stanford Health Care – November 2017
by Jason A. Wolf, PhD, CPXP
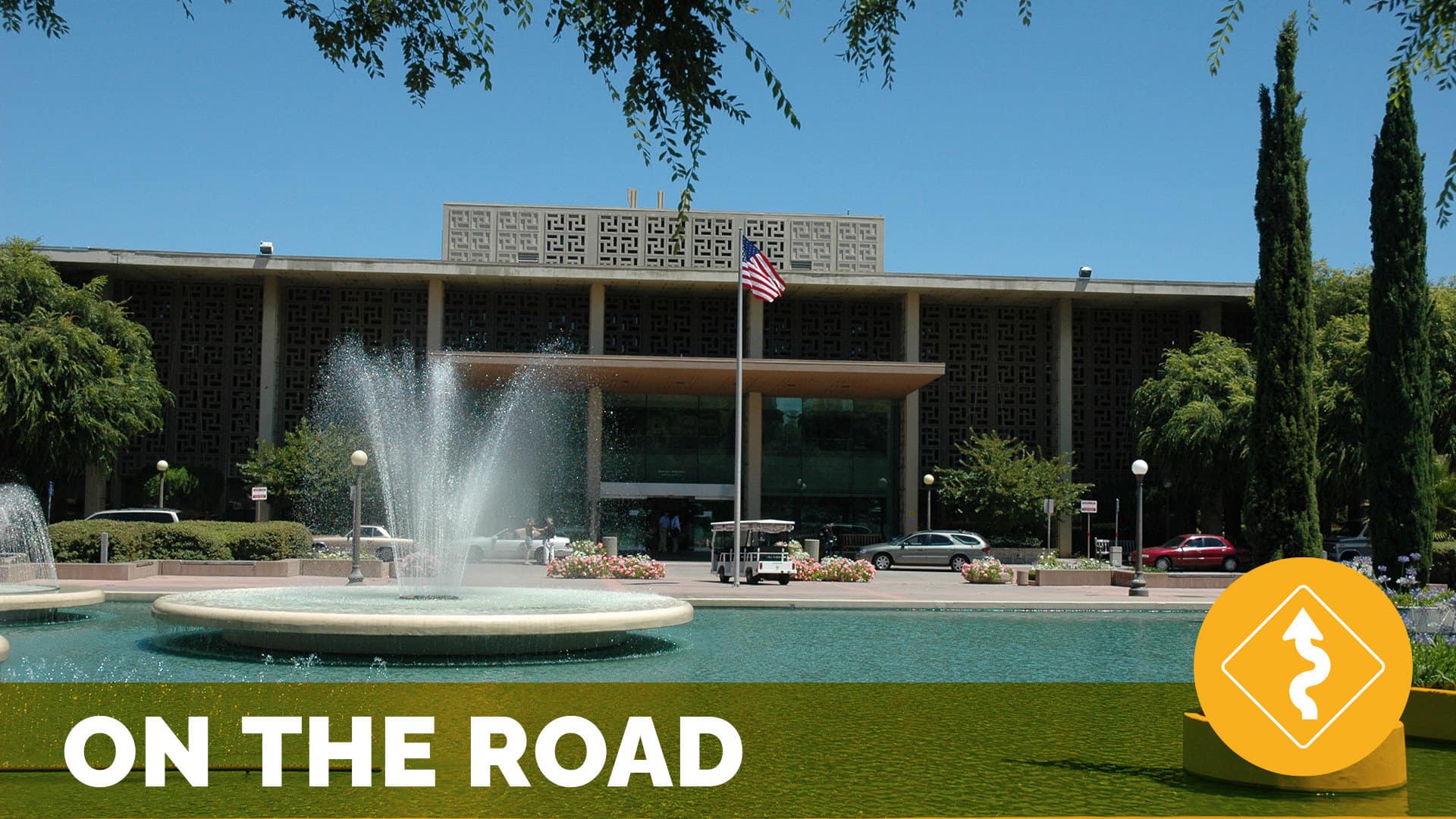
Our latest On the Road took me to Stanford Health Care. I arrived to a scene of early morning healthcare bustle, the sounds of a construction site for the new facility just awakening and creaking its sleepy bones, the transition of students from academics to practice and the calming sense offered by a reflecting pool and fountain tying you back to the earth. This intersection of senses, the weaving together of our intricate healthcare world would in a way epitomize the day I was about to spend with the Stanford team. In our dynamic healthcare world today, my visit showed me a thoughtful and conscious effort to integrate an institution committed to health into a center that helped bolster the very human experience in its midst.
At The Beryl Institute, earlier this year we shared an expanded perspective that has emerged from our work over the last seven years in digging into and working to expand the patient experience movement. This perspective was further pushed by the very findings we shared in our most recent State of Patient Experience study, highlighted by the fact that employee engagement was the fastest growing and now top priority for those tackling patient experience improvement. The idea – that at the heart of healthcare we must ensure an unwavering commitment to the human experience – was exemplified in the comprehensive effort to address experience that Stanford shared. My hosts, Bryanna Gallaway, Director of Service Excellence, Mysti Smith-Bentley, Administrative Director of Service Excellence and Alpa Vyas, Vice President of Patient Experience provided me a powerful view of how Stanford Health Care was working every day to ensure this focus remained central to their work. At the core of their effort was the C-I-CARE program.
C-I-CARE: Actively Managing for the Human Experience
I was first introduced to the C-I-CARE process in 2011 during an On the Road visit to UCLA. What I experienced in my time at Stanford was a purposeful evolution of this program now at the heart of Stanford’s effort. I want to note up front as well that as much as C-I-CARE serves as an acronym regarding how people should communicate, it is the rigor of the broader process behind its intentionality that drives its biggest impact. As the Stanford Health Care materials on C-I-CARE describe: C-I-CARE is a framework for structuring best practice communications and developing relationship-based care approaches with patients, families, and our colleagues. It is our standard work for ensuring we provide the best patient experience anywhere, period!.
My notes from the visit included a personal comment that as much as I hoped to convey the power of this process in this story, you have to experience it to fully capture the essence of the work (and I encourage you to do so). I offer two links to handouts that more succinctly provide a one sheet overview to C-I-CARE as well as the resources and processes at the disposal of leaders at Stanford Health Care. The key elements of this effort include a commitment to onboarding and training, a focus on active daily management, and a commitment to ongoing support. It is driven by not just the communication framework it represents, but in four core practices – telephone etiquette, wayfinding, C-I-CARE with colleagues and service recovery.
What is significant in the model is that as a strategic framework it gives purpose to both consistent process and the application of core tactics with meaning. Implementing a system like this, while not easy has longer lasting effects that the simple adoption of tactics with no structure of support. This is a lesson I believe many organizations have learned as they have attempted their own experience improvement efforts. Improvement efforts implemented on a poor foundation don’t seem to ultimately result in, let alone sustain the results many aspire to achieve.
During my visit, I had the opportunity to experience the tiered huddles that are part of the active daily management process. This structured, timed and purposeful effort ensures that work efforts were clear, staff location (literally where they were that day) was understood and issues to address were raised as the conversation moved up the tiers. From the front lines of managing service excellence, patient complaints and volunteer services are just a few examples I experienced on how these teams worked to share and understand not only the work they had at hand, but anticipate the issues and opportunities that might arise. The roll-up of issues moved level to level as I watched in real time problems acknowledged and addressed all while a shared sense of understanding and awareness was generated.
In the midst of the management process was also another clear element. It wasn’t solely about the “work of healthcare” it was about those who worked in it as well. These huddles became opportunities for recognition and celebration, for learning and sharing and created a strong sense of not just team, but a bond linked to purpose which was evident. In my opportunity to watch the tiers role all the way up to the C-Suite you saw how each function, from facilities to clinical excellence, IT to experience also came together to align and understand efforts to ensure focus, awareness and the ability to respond with speed and agility.
Key to this effort wasn’t just the work discussed, but in my observation these efforts were about sharing the stories of the organization, reinforcing its strengths and identifying its opportunities. One story I was told was about “Randy” and the power of team communication and management. The story is about a patient coming in for a procedure one day and she was nervous and anxious about what was ahead. As part of her registration she was told, “Oh, great news, Randy is on the schedule today”. Then at almost every step in her care journey she kept hearing about Randy from intake to prep. He sounded amazing and she ultimately had to know who this Randy was. When she finally met him – he was the tech for her procedure – she was feeling calm and confident. How could she not be, she had Randy. This level of connection, shared support and aligned understanding is central to this process at Stanford Health Care. In fact, it was reinforced in my conversations with another unique element Stanford put in place, the Service Medical Director Team.
Actively Managing for Physician Engagement
One of the unique aspects of Stanford’s effort and one I will start up front by saying is something every organization should consider was exemplified by the Service Medical Directors. In almost every encounter I have with a healthcare organization the question on physician engagement and how best to tackle it comes up. The model Stanford has had in place now for the last seven years has done much to tackle this issue. The experience team created a physician steering team of some of the top physician leaders in the organization to help reflect on and champion the efforts they were taking on.
As one member said, “When we started this journey there was resistance as expected and as we came to see and helped convey the ideas behind C-I-CARE were not just soft skills, but practices that are central to good quality care.” He added, while Stanford historically had a reputation for being technically proficient it was lacking in the area of human experience. What we came to see and support was our ability to make this place more human.”
This idea of a team of leading physicians as champions is not novel, but it is not easy. The team represents in many ways what other organizations have attempted through identifying physician champions. Again, this reinforces it is not just applying the tactic that made the difference for Stanford, but it was the operating foundation on which the effort was built.
As one of the team members offered, “When you walk into the hospital now under C-I-CARE it is a much different place.” Another member said, “C-I-CARE was transformative. It helped us see the human beings on the other side of the door. It changed the interactions between us and our patients AND between one another.” She then added, “C-I-CARE has become a fundamental part of our culture – it is now a noun, a verb and an adjective!” And another team member agreed by saying, “It was easy to champion this effort as it was something that was clearly and purposefully for everyone.” It was evident as a team of champions they had bought into the idea, but more so they reinforced how they were both a conduit and exemplars on how and why this was a critical focus for the organizational overall. It was impacting outcomes and touching lives.
In asking Alpa Vyas about her thoughts on the team, she simply added, “My piece of advice for anyone trying to drive experience excellence is to create a group like this.” She noted how instrumental the team has been in changing the conversation and engaging physicians in ways that they had not been before. They tackle opportunities and provide feedback, they review data and survey replies and address tough issues that arise. And with this the team acknowledged one thing as well. This team and its intention made a statement to the medical staff as well. That their voices matter and they can be champions and owners of this work.
C-I-CARE Rounds: Elevating Champions at All Levels
As part of my visit I had the chance to attend C-I-CARE rounds. An all leadership monthly effort to introduce the key points of the month, intentionally round on various units and departments across the system and share some of the critical findings for shared learning and improvement. As I said early, these are events to be experienced and don’t get their full justice in words on a page. With that the spirit that was generated from this full leadership rounding process was palpable. In fact, the event I was attending during my visit was not just rounds, but literally a kick-off pep-rally for the year ahead.
The process for these rounds is a shared learning opportunity, in the instance of my visit it was the introduction of the StoryCorps partnership at Stanford Health Carewhere they were capturing patient, family, and colleague stories in their midst. The example shared that morning was from a nurse and a powerful encounter she had that reinforce to her why she became a nurse and took on “the hardest job you’ll ever love”.
From initial shared comments, the 1000 plus leaders at all sites across the Stanford system head out to round at assigned locations. This is done not just on the main campus, but the groups are connected via video and phone from around the Bay Area. I had the chance to round on a neurology/stroke unit with an incredible nurse leader, Shirley Weber, Vice President of Clinical Operations. We had the chance to ask a few questions assigned for the rounds that day and more so I was able to find out from nurses on the front line of care about their perspectives on the C-I-CARE process overall. They shared they their unit was growing stronger as a team and as a “family” and that C-I-CARE framed a strong process for them to engage and share ideas. She highlighted how it enabled them to close the loop, take action and share learning.
During my rounds, I also had the chance to visit with a patient on the unit to better understand her experience and what mattered to her. It was almost as if planned, as I posed the question to her about what stood out in her experience at Stanford her nurse happened to enter the room and the patient pointed to her, smiled and said, “That nurse right there!” This reinforced above all else that in creating processes we don’t take the humanity out of care, but in fact can reinforce and ensure it is addressed, if we do so with purpose. This is what I found at Stanford Health Care.
As we reconvened to close out rounds, the team shared highlights and stories with one another on what they saw, points of excellence and kudos, and opportunities to improve. It felt as if in almost every encounter I had at Stanford there was not only a commitment to excellence, but a commitment to improvement, to learning and getting better at every opportunity that presented itself. The debrief played a critical role in sharing stories, celebrating success and tackling immediate issues. And everyone was engaged in the process.
This collective alignment to outcomes reinforced ideas that have been central to the definition of experience since our start at the Institute – that it occurs through interactions and is shaped by the culture of an organization. The bottom line is the people an organization puts in place and the resources and skills they put at their disposal are as critical to experience outcomes as anything they can do.
An Unwavering Commitment to the Human Experience
Reinforcing the role of people in the organization I had the chance to meet David Jones, Chief Human Resources Officer and Todd Prigge, Administrative Director of Training & Organizational Development. I have long believed in the role HR plays in the overall experience, from acquiring the talent to deliver on an experience promise, to delivering the skills needed to execute on and sustain results. This was evident in the vision and the strategic HR efforts for Stanford Health Care. As David reinforced, “We want to be known for the experience we provide. In order to do that we must ground our efforts in our own employee experience.” This idea was reinforced in the State of Patient Experience data I shared above. It also exemplifies the clear commitment in Stanford’s efforts as seen in the “four cores” of C-I-CARE in caring for colleagues.
As David added an effort such as C-I-CARE is not just a process you implement, it is a significant and weighty culture change effort. And in fact, was a rapid and highly impactful culture change effort overall. This takes the strategic alignment of people in all corners of the organization who understand and are willing to engage in the effort. As he reinforced, “every interaction matters.”
This idea of the power of interactions was reinforced as I had the chance to spend time with Stanford Health Care’s Founding Patient & Family Advisory Council (PFAC). Stanford now has 16 active patient and family partner groups engaging over 142 individuals (you can see the full report on their impressive Patient & Family partner via this link). My chance to meet with this group and the team led by Mary Song, Manager of Volunteer Resources, earlier in the day committed to engaging not just patient and family partners but the 1000s of volunteers helping Stanford reinforced the importance that Stanford places in its process from hearing and honoring all voices. The conversation that took place at the PFAC dinner addressed some critical opportunities for improvement and engaged in a review of strategy for 2018 to gather input on the plan. It was also clear that while this was a standing meeting this committed team of volunteers took their work seriously in understanding, engaging in, pushing at and supporting the efforts at Stanford Health Care. As one member told me as we wrapped up the meeting, “this is one of the few boards like this I have been on where I feel like we get to tackle real issues and our voices matter in the actions that are taken as a result.” That is the essence of human experience…that all voices matter.
A Chance to Learn from One Another
I am always humbled by the chance to visit great work happening in healthcare around our world and by the unwavering commitment by which so many tackle this noble work. The efforts at Stanford exemplify this reality and reinforce a point I so often write in these pieces, that an article can never fully convey the experience an organization is ultimately offering or share every intricacy of their efforts. What I didn’t share here, but is worth learning more about is the intricacies behind operationalizing C-I-CARE and more so what is beneath it. The very infrastructure for experience at Stanford that was shared by Alpa and her team show an incredible infrastructure of departments and services, from call centers to service recovery, that all have a critical role to play in experience excellence. For this reason, as much as I can convey a visit, I encourage organizations to spend time with one another as well and am excited to see more of this happening every day.
With that, we are excited to see some efforts afoot among our boards at the Institute and soon with our input to look at what a more formal visitation program to learn about one another’s experience efforts could look like in concept and reality. It is commitment to connection and sharing that remains the truly unique and powerful essence of our work and of our community at The Beryl Institute.
This commitment to connection and sharing, with a focus on actions and outcomes was also found at the heart of all I experienced during my visit to Stanford Health Care. The structure and rigor of the work to ensure the best in human experience is hard to escape. And even though not always easy work, Stanford Health Care has made it top priority for all they do. It’s the breath of the organization, it is felt in its heartbeat and exemplified in its choices and actions.
As part of my visit we were also honored to have Stanford host one of our 2017 Regional Roundtables which provided many others regionally the opportunity to experience their efforts. One of the speakers was Kristen Terlizzi, a patient partner from Stanford with a powerful and palpable story about how the Stanford experience impacted her life. It was in her closing remarks that she may have best summarized what the efforts at Stanford made possible. “We may not be able to control the world, but we all have the ability to impact the human experience!”. That is what the efforts at Stanford Health Care have ensured for all in their system – staff, volunteer and patient/family member alike – the ability to impact the human experience. And it is clear it is something they are committed to each and every day.
Related content
-
 Culture & Leadership
Culture & LeadershipBroaden the Scope of What You Consider Experience
Stacy Palmer, Senior Vice President & COO of The Beryl Institute, sits down with Pattie Cuen, Senior Vice President of Jarrard Inc., to discuss a recent consumer survey about public values in healthcare experience. Listen in as Cuen shares key insights and emphasizes the importance of seeing the bigger picture of experience by focusing on
Learn more -
 Culture & Leadership
Culture & LeadershipYCX: How Three Letters Impacted Culture, Engaged Leaders, and Drove Results
By Brent A. Grunig, Communications & Training Consultant, The Southeast Permanente Medical Group The Southeast Permanente Medical Group (TSPMG) named 2023 as the “Year of Care Experience”— or YCX. What started out as an idea for a year-long campaign ended up becoming an overwhelming success using a multi-faceted approach across teams and departments within TSPMG
Learn more -
 Culture & Leadership | Infrastructure & Governance
Culture & Leadership | Infrastructure & GovernanceCrafting a Patient Experience Program While Commissioning a Hospital
Global Headliner Webinar Series (Complimentary) – Whether you’re building from the ground up or refreshing your current approach, join this webinar for practical guidance for making patient experience an integral part of your organizational culture. • 12:00 PM AST (Arabia Standard Time) • 5:00 AM EDT (Eastern Daylight Time – New York) • 9:00 AM
Learn more
