The Power of Connection: Celebrating Community
On the Road at our first 10 Roundtables – October 2015
by Jason Wolf, Deanna Frings and Stacy Palmer
Every fall members and guests of The Beryl Institute gather at Regional Roundtable events to network and share best practices around patient experience improvement. Since the program began in 2011, ten of these events have occurred, each slightly different in dynamics and outcomes but all sharing the commonality of passionate people working together to drive experience improvement. These one-day meetings are intended to energize and educate participants and prepare and motivate them to tackle the patient experience challenges at their individual facilities.
Roundtables are hosted by members of The Beryl Institute who graciously open their facilities to provide meeting space and recruit staff members to help ensure a great event. The day is bookended by two keynotes speakers who set the tone and provide valuable perspectives and inspiration.
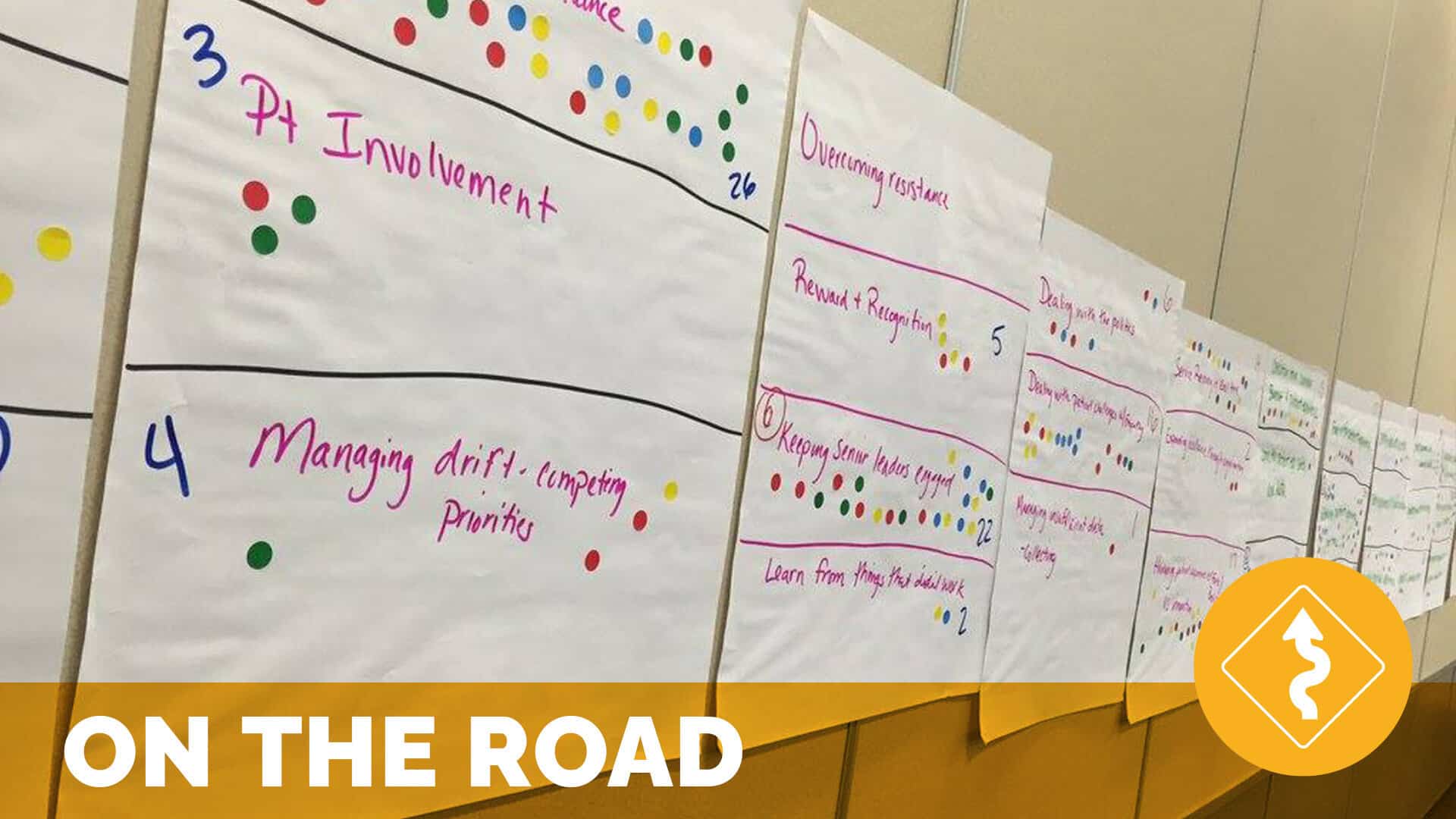
In between the two keynotes lies the hands-on, interactive sessions that truly makes these events unique. Participants identify topics for discussion onsite through a group brainstorming activity where they are asked to share their top patient experience priorities. Participants collectively develop a list of potential discussion topics and then are each given a strip of round stickers and asked to vote using the stickers on the topics they are most interested in exploring together. The top six choices become the table topics for the day and participants rotate among the tables for discussion with peers.
The combination of keynote speakers, working group sessions and even an optional facility tour from the site host makes for a full day, but participants continue to share their appreciation for both the formal program and opportunities to meet other passionate patient experience professionals. These events exemplify the one underlying and powerful philosophy that drives our work at The Beryl Institute. It is through the collective voices comprising our global community of practice that we generate ideas, learn and share with others.
2015 ROUNDTABLES
Our 2015 travels took us to three great cities and wonderful hosts; first to San Francisco and host organization UCSF Health, then Charlotte and host organizations Carolinas Healthcare System and finally to Minneapolis and host organization Allina Health. The purpose and format of our events continued to hold true with both strong messages from insightful keynotes to rich conversations with peer groups in addressing the pressing issues impacting and influencing patient experience today. In 2015, we were also excited to ensure that a patient or family member voice was one of the keynote speakers for each event. We share some of the headlines from this year’s gatherings below.
UCSF Roundtable
The roundtable in San Francisco was framed by two powerful presentations pushing us to think and act differently in addressing the patient experience. Opening keynote Randi Oster reinforced the need to engage patient and family members in their care process and stressed the critical importance of the willingness to listen. More so she offered that in truly achieving patient experience success we must not only understand the patient’s emotional needs, i.e. what motivates or moves them, but also we must design our efforts with that emotional end frame in mind. This was a powerful example of simply engaging patients to integration their perspective in action.
Our closing keynote Jake Poore stressed critical points as we work to build overall patient experience efforts in our organizations, suggesting that while the underpinnings of patient experience are common sense, they are not common practice. He stressed our job in healthcare is not service, but rather the removal of trepidation and anxiety, of as he suggested, “caring out loud”. In acknowledging that our organizations have a culture that impacts the overall experience whether we create one or not, he offered that there is great power in the stories we create and tell leaving us with a profound idea in supporting our work “you better tell your own story, or others will tell it for you”. This left many to think about what their organization’s patient experience story should be.
The heart of the day in San Francisco took us through the open discussion of participants on the issue they deemed most pressing for them. The top six topics identified included innovations in patient experience, behavior change, organizational strategy, staff engagement, physician engagement and health literacy. In each round of discussion, the practices and opportunities in addressing these ideas were expanded, the key headlines of each theme included:
Innovations in patient experience. We have to realize innovations are more than technology and with the push for innovation must still remember we are working with people.
Behavior change. Identified as a central challenge and opportunity driving patient experience success the core idea emerging was that leadership must not just stress expectations, but model and have the willingness to reinforce this in time, dollars and people efforts.
Organizational strategy. As people acknowledged the importance of experience as central to strategy in healthcare today a powerful point offered was that experience must have a clear and convincing mission, purpose and focus that is authentic, memorable, translatable and easy to communicate. This is about building and sustaining the types of culture through which we will deliver our services.
Staff engagement. A poignant reminder in the importance of team engagement was we should be treating our staff the way we would expect our patients to be treated.
Physician engagement. This topic remains an item of interest and focus annually and suggests we still have work to do on this topic. The simple ideas remain. We must work to collaborate with physicians through engaging them as contributors, not simply executors of process. We must also not just engage, but recognize and even incent physicians in ways that support and motivate them to action.
Health literacy. As this topic emerges, it reinforces that we must think of our healthcare language from the end-user perspective. Rather then teaching people up to our current healthcare terminology, how do we make our terminology more accessible and understandable to patients and families?
Carolinas HealthCare System Roundtable
The conversation continued in Charlotte again with two thoughtful and passionate speakers focused on framing ideas in support of strong and successful experience efforts. Our opening keynote, Bernard Roberson shared the power of patient and family engagement suggesting that patients and families are the best asset in improvement, offering, “When we invite patients and families to be partners in their care, outcomes improve. It’s really that simple.” He reinforced the true power of perception in saying that we are not hiding anything patients and families don’t already know.
Our closing keynote, Tiffany Christensen, ended the roundtable to a standing ovation in sharing not only her personal health journey but also how it has turned her into a contributing player in healthcare improvement. She offered that to engage people successfully in experience efforts we need to first recognize the power of partnership that it takes and then inspire action not just by stating expectations, but motivating action through the power of story. This underlined her point that for as much as we need processes to cross our efforts in healthcare, we must also recognize the individuality of those we care for. We must see the person in the room or bed and understand that every person is unique.
The framing conversations again shaped the central discussion of the day around the identified topics of accountability, physician/provider engagement, integrating patient experience, measuring beyond CAHPS, PX in the emergency department and explaining so patients understand. The key headlines of each theme included:
- Accountability.We must move our conversations beyond blame to focus on resolution. With this we are creating ownership by supporting participation. This is beyond fixing issues to working proactively to drive solutions in advance of the problems we foresee.
- Physician/provider engagement. A repeat topic and trend in the roundtable discussion, the group in Charlotte raised the issue of transparency and monthly reporting as a means to support engagement. They also addressed the importance of hiring those who are aligned with the values and intention of the organization from the start.
- Breaking down silos/Integrating patient experience. The group offered that experience must be focused on and intentions in crossing and aligning efforts across organizational silos. PX leaders must be focused on building relationships, education (both formal and informal) and creating champions across the organization to extend their team and reinforce key efforts and messages.
- Measuring beyond CAHPS. The discussion acknowledged the lag of current measures to address the immediate needs their organizations faced and suggested we must find ways for better and more immediate feedback. We must find ways to engage voice in real time via rounding, bedside surveying, etc. and work to educate leadership that PX is much more than just CAHPS scores.
- PX in the emergency department. While this could be a full conference unto itself, the groups dug in to address this issue. The key idea that emerged was that while EDs are often chaotic and critically focused, they still have the opportunity to begin and end encounters with the broader perspective of care in mind. In looking at better processes for interaction and communication with those who enter EDs there is great opportunity for experience improvement.
- Explaining so patients understand. A variation and emerging theme in line with the health literacy discussion we had in San Francisco, the discussion touched on the importance of ensuing there was a clear means to assess and generate awareness of patient and family understanding and awareness. We can and should work to simplify, explain and involve people in the conversation. This not only creates a better experience, but also can lead to better outcomes overall.
Allina Health Roundtable
Allina Health in Minneapolis hosted our final 2015 Regional Roundtable. The day started and ended with a critical reminder from our keynote presenters; that the success of delivering a high-quality, safe and positive patient experience lies in our own success of understanding, appreciating and addressing the fears and concerns of the patients and families we serve.
Our opening keynote, Colleen Sweeney, ignited the group as she shared her experiences and personal journey that led to the Patient Empathy Project, a 3 1/2-year study exploring what patients fear most about hospitals, healthcare and doctors. The gift she offered was tangible solutions on how to identify and address those fears and concerns and was grounded in her own experience as a critical care nurse. She shared her key lesson; that the most important thing she had to offer her patients was not her technical competence, but her willingness to pay attention to those fears and concerns.
Our closing keynote, Matt Cavallo’s story telling brought us full circle to where the day began. His experiences as a young man living with multiple sclerosis illustrated the critical impact of his unaddressed fears. His gift was giving us the opportunity to empathize with and learn from his experiences. He closed with a powerful and appreciative note of thanks and affirmed an important message. That the patient experience is truly the sum of all interactions shaped by an organization’s culture that influence patience perceptions across the continuum of care.
The roundtable discussions again filled the heart of the day, this time around the identified topics of hardwiring excellence, capturing the hearts of staff, physician engagement, including patients and families on project teams, culture change and accountability. The key headlines of each theme included:
A large portion of the day was spent in interactive conversation. The key themes and headlines included:
- Hardwiring excellence.Sustaining efforts in patient experience excellence requires as much attention and focus as generating solutions. A key recommendation that emerged was less is more. Limiting the number of solutions implemented at any one time has demonstrated greater long-term success and sustainable results.
- Capturing the hearts of staff. Emerging from the discussion was a list of ways to recognize staff for the work they do every day. This simple principle is a powerful way to connect the “what” we do with the critical importance of “why” we do it. Recognition is an impactful way to achieve engagement at all levels.
- Physician engagement. Not surprisingly, this common theme again appeared. A central idea offered is to begin with an appreciation of what physician’s value most about a positive patient experience. After this initial exploration, the invitation to participate should also include education, tools and strategies to support their success.
- Including patients and families on project teams. Multiple examples and logistical details of how to engage patient and family involvement were shared. This strong focus on engagement reminds us that we are experiencing an exciting paradigm shift in recognizing that the inclusion of patients and families in shaping the delivery of care is more the norm today. The lesson was simple, if you don’t do this in your organization, you must.
- Culture change. Recognizing that changing a culture can be an overwhelming task to take on, a poignant idea generated was the idea of implementing small tests of change. Rather then becoming captive to resistance, show small victories to gain buy in and momentum.
- Accountability. Many things were included in the discussion on accountability. In summary, having clarity on purpose, setting clear expectations and driving individual ownership will go a long way in establishing a culture of accountability and as a result achieving desired outcomes.
EVOLVING TRENDS
At the heart of the Regional Roundtable events have been the open and active discussion on the priorities for action in patient experience performance and improvement. In asking each group what their critical priorities were, we can now see both a consistency in opportunity and an evolution in focus over the last five years. With the first event being held in November 2011 and the most recent just concluding this month, we have a line of sight into how the patient experience conversation has progressed.
The themes have grown over the year with some consistent underlying priorities since the start. There has also been a macro shift from a focus driven by the emergence of HCAHPS to more recently a broader strategic intent. There are eight major themes that have paved the journey and provide us both a picture of ongoing opportunity for action and a refocusing point on the direction patient experience work is moving.
The most popular themes, listed in the table below are presented with both the number of roundtables in which they were identified as a priority and also the date range in which they were addressed. The themes and headlines include:
Theme # of Mentions
(max 10) Years
Physician Engagement 8 2011 on
Accountability 6 2011 on
Culture 5 2011 on
Patient & Family Engagement 5 2013 on
Employee Engagement 4 2013 on
Sustainability 4 2013 on
Breaking Down Silos 3 2014
Health Literacy 2 2015
What this analysis revealed is telling. From the beginning and continuing through today, organizations are struggling to address physician engagement, ensuring staff/team accountability and building/reinforcing the type of culture needed to positively perform in patient experience. These trended priorities also suggest some of the core ideas we see as fundamental to patient experience success, ensuring physicians understand the importance and value of experience, reinforcing the critical nature of the role all people play and creating an organizational and strategic framework to support and sustain efforts.
From this point we see an evolution away from the tactics of address specific HCAHPS domains to working fundamentally on the ideas that support those first three broader issues. In 2013 we see both patient & family engagement and employee engagement hitting the radar screens in greater volume, with the focus on not just building but sustaining efforts now top of mind. Thinking further evolved as in 2014 we observed the extended conversation on how we break down silos to ensure a broader and collective conversation on experience excellence. Finally, just this year with the discussion of health literacy an emerging awareness has been seen in how we engage and communicate with patients and families in order to make their care experience accessible to them.
These are exciting and significant trends as they show both the continued struggles organizations are tackling, while at the same time reflect the depth at which they now acknowledge they must go to provide the best in patient experience. These trends help us see that many have moved beyond simply addressing survey results to focus on the organizational fundamentals of engagement, communication and the integration of efforts in driving outcomes. These findings are of great excitement for us at The Beryl Institute as they parallel the very ideas and information we have both come to see at work and have come to espouse as critical to patient experience success. They also provide a great framework to test your own organization’s focus and progress and provide an insightful roadmap into how we can and should be evolving as healthcare organizations to ensure the best in experience for all engaged.
POWER OF CONNECTION
As we talked of the intent of the Regional Roundtable as part of what we do at The Beryl Institute in being a true community of practice, you can see in the three examples from this year and the emerging trends that there is powerful, significant and actionable knowledge available when we gather as peers, share out ideas and walk away with that next idea of nugget for action. While we may not always have the opportunity together physically as we did in these events, we strive every day at The Beryl Institute to not just provide access to information, but to support the connection among all members of our community. We encourage you to continue these types of conversations with your peers in linking as members of our community, engaging or even suggesting a new special interest community, coming together next spring at Patient Experience Conference or again next year at our 2016 roundtables.
The opportunity we have in patient experience improvement is to realize it is a shared journey. That may be one of the biggest lessons learned through these first 10 roundtables. In coming together, we can accomplish amazing things. We are honored to support this journey and be a home for this critical focus in healthcare. We invite you to continue this adventure with us and to encourage others to come along. There is still much as can and will do together.
Related content
-
 Infrastructure & Governance
Infrastructure & GovernanceRebuilding Trust to Ensure Sustainability: One CAH’s Remarkable Transformation
On the Road with Phillips County Health Systems – August 2019 by Tiffany Christensen, CPXP When The Beryl Institute Team goes On the Road, some trips include more “road” than others. Getting to Phillipsburg, Kansas required 3 planes, a rental car and a long drive through miles of farm country. Getting the opportunity to learn
Learn more -
 Infrastructure & Governance
Infrastructure & GovernanceGoing Off on a Tangent: Exploring the Possibility of Process Change
Most people are familiar with the quote by the Greek philosopher Heraclitus, “Change is the only constant in life.” As wise and true as these words are, change still catches most of us by surprise. In some people, the fear of change can even be anxiety-provoking (a condition known as metathesiophobia). While most of us
Learn more -
 Infrastructure & Governance
Infrastructure & GovernanceService Recovery for All: The Out-Patient Setting
Those working in healthcare have been experiencing the challenges associated with incivility of patients and family members. The workforce needs tools to effectively and confidently have conversations with upset individuals.
Learn more
